Before euthanasia or assisted suicide is legal, the whole debate is about people who are in grave pain yet completely in their right minds. The proponents talk about people who are terminally ill and just want to end their suffering.
Once it is legal, we see how often euthanasia becomes a very slippery slope happens otherwise. In some cases, the person didn’t clearly have a full mind or didn’t clearly consent. In other cases, it is a calculation of how much less it costs. In still others, it seems like a form of eugenics.
During initial debates, the opponents warn of a slippery slope where euthanasia happens in particularly problematic ways. Proponents dismiss this as scare-mongering when we first debate such legislation. However, the evidence that this slope exists comes with the laws in force. Here I want to compile some of that evidence. Euthanasia is bad, but the slippery slope always makes it worse.
(Note: In assisted suicide, unlike euthanasia, the person who dies administers the drugs. However, fundamentally both go against the Hippocratic principle of “do no harm.” All said here can apply to both.)
Examples of Euthanasia and Assisted Suicide
A Dutch Autistic Man
The New York Post offers the case of an autistic in his 30s.
In early childhood, the Dutch psychiatric patient known as 2014-77 suffered neglect and abuse. When he was about 10, doctors diagnosed him with autism. For approximately two decades thereafter, he was in and out of treatment and made repeated suicide attempts.
He suffered terribly, doctors later observed, from his inability to form relationships: “He responded to matters in a spontaneous and intense, sometimes even extreme, way. This led to problems.”
A few years ago, 2014-77 asked a psychiatrist to end his life. In the Netherlands, doctors may perform euthanasia — not only for terminal physical illness but also upon the “voluntary and well-considered” request of those suffering “unbearably” from incurable mental conditions.
The doctor declined, citing his belief the case was treatable, as well as his own moral qualms. But he did transmit the request to colleagues, as Dutch norms require. They treated 2014-77 for one more year, determined his case was, indeed, hopeless and administered a fatal dose of drugs.
The story goes on to show a wider problem.
According to an analysis of 66 of the 110 cases [of euthanasia for a mental disorder] from 2011 to 2014, by psychiatrist Scott Kim of the National Institutes of Health and two colleagues, Dutch psychiatric patients were often euthanized despite disagreement among consulting physicians as to whether they met legal criteria. In 37 cases, patients refused possibly beneficial treatment, and doctors proceeded anyway.
The Kim report, published Feb. 10 in the journal JAMA Psychiatry, undercuts the very notion of a “voluntary and well-considered” request for death from a patient who is, by definition, cognitively and/or emotionally troubled.
A Belgian Woman After Breakup
Another woman in Belgium was euthanized at 38 because she felt extremely distraught after a romantic breakup. A Belgian website quoted from her sisters’ interview on TV.
To get euthanasia, three doctors must give their permission. According to the sisters of Tine, she chose the doctors themselves and they did not exchange information with each other. “Furthermore, someone must have an incurable mental illness for euthanasia based on psychological suffering, and Tine did not.”
“The doctor who performed the euthanasia was nonchalant to say the least”, they then put their finger on a wound that still pricks today.
“He compared her death to that of a pet who suffers and receives a syringe, and he did not have the necessary equipment, he laid the mixture with the deadly liquid next to her on the chair. While she was dying, the plastic bag fell on her face.”
“He also asked our father to hold the needle in her arm because he had forgotten to bring plasters, and when she died, he asked our parents if they would listen to the stethoscope to check that her heart had stopped to beat.”
November 27 update: the doctors are being prosecuted for unjustly euthanizing her. BioEdge reports:
For the first time in the history of Belgium’s euthanasia law, doctors have been arraigned before a court for breaking it. This week a court ruled that two doctors and a psychiatrist from the province of East Flanders had illegally assisted in the euthanasia of a 38-year-old woman suffering from autism in 2010.
Tine Nys was euthanized on April 27, 2010 on the basis of mental suffering. Her sisters complained that the doctors acted incompetently and failed to observe the letter of the law.
A court in Ghent found that there was sufficient evidence that the conditions and procedures of the Euthanasia Act had not been observed. The three doctors, including a psychiatrist, will be arraigned for poisoning.
Study of Data Regarding Euthanasia on NIH Site
The NIH (National Institutes for Health – your tax dollars at work) posted a study online about how the safeguards in European countries with legal Euthanasia have failed. They also include some details about Oregon’s assisted suicide laws, despite the Eurocentric focus. Here are a few key passages.
In all jurisdictions, the request for euthanasia or PAS [Physician Assisted Suicide] has to be voluntary, well-considered, informed, and persistent over time. The requesting person must provide explicit written consent and must be competent at the time the request is made. Despite those safeguards, more than 500 people in the Netherlands are euthanized involuntarily every year. In 2005, a total of 2410 deaths by euthanasia or PAS were reported, representing 1.7% of all deaths in the Netherlands. More than 560 people (0.4% of all deaths) were administered lethal substances without having given explicit consent. For every 5 people euthanized, 1 is euthanized without having given explicit consent. Attempts at bringing those cases to trial have failed, providing evidence that the judicial system has become more tolerant over time of such transgressions.
In Belgium, the rate of involuntary and non-voluntary euthanasia deaths (that is, without explicit consent) is 3 times higher than it is in the Netherlands. (“Involuntary euthanasia” refers to a situation in which a person possesses the capacity but has not provided consent, and “non-voluntary euthanasia,” to a situation in which a person is unable to provide consent for reasons such as severe dementia or coma). A recent study found that in the Flemish part of Belgium, 66 of 208 cases of “euthanasia” (32%) occurred in the absence of request or consent. […]
Reporting is mandatory in all the jurisdictions, but this requirement is often ignored. In Belgium, nearly half of all cases of euthanasia are not reported to the Federal Control and Evaluation Committee. Legal requirements were more frequently not met in unreported cases than in reported cases. […]
The involvement of nurses gives cause for concern because all the jurisdictions, with the exception of Switzerland, require that the acts be performed only by physicians. […] Nurses performed the euthanasia in 12% of the cases and in 45% of the cases without explicit consent. In many instances, the physicians were absent. […]
All jurisdictions except for Switzerland require a consultation by a second physician to ensure that all criteria have been met before proceeding with euthanasia or PAS. In Belgium, a third physician has to review the case if the person’s condition is deemed to be non-terminal. The consultant must be independent (not connected with the care of the patient or with the care provider) and must provide an objective assessment. However, there is evidence from Belgium, the Netherlands, and Oregon that this process is not universally applied. In the Netherlands, for example, a consultation was not sought in 35% of cases of involuntary euthanasia. In 1998 in the Netherlands, 25% of patients requesting euthanasia received psychiatric consultation; in 2010 none did. Moreover, non-reporting seems to be associated with a lack of consultation by a second doctor.
In Oregon, a physician member of a pro-assisted-suicide lobby group provided the consultation in 58 of 61 consecutive cases of patients receiving PAS in Oregon. This raises concerns about the objectivity of the process and the safety of the patients, and raises questions about the influence of bias on the part of these physicians on the process. […]
Oregon requires that a patient be referred to a psychiatrist or psychologist for treatment if the prescribing or consulting physician is concerned that the patient’s judgment is impaired by a mental disorder such as depression. In 2007, none of the people who died by lethal ingestion in Oregon had been evaluated by a psychiatrist or a psychologist, despite considerable evidence that, compared with non-depressed patients, patients who are depressed are more likely to request euthanasia and that treatment for depression will often result in the patient rescinding the request. In a study of 200 terminally ill cancer patients, for example, the prevalence of depressive syndromes was 59% among patients with a pervasive desire to die, but only 8% among patients without such a desire. Despite that finding, many health professionals and family members of patients in Oregon who pursue PAS generally do not believe that depression influences the choice for hastened death.
The scariest part of that information is that most of those studies are relatively old and as euthanasia or assisted suicide gets more common, I would suspect safeguards are less strictly enforced.
The USA is not exempt from these problems. To summarize the problems with Oregon’s law according to that study: zero received psychological evaluation despite depression and the desire to die being highly comorbid, many lacked the second physician, and pro-euthanasia lobbyists handed out 95% of the drugs. The Oregon state health department’s report on cases notes that some people have a relationship of 0 or 1 weeks with the physician who prescribes the drugs. The median was only 13 weeks from 1998-2014. I don’t know about you, but 3 months seems a rather short time to be with a physician. It’s all-the-more-brief if we consider that these physicians are signing off on lethal drugs.
Misrepresentations of the Data in the Media
Unfortunately, the media tends to miss this in their reports. For example, The Economist writes the following uncritically.
Kim Callinan of Compassion & Choices, a pressure group, believes there are several reasons for the growth in support. Since the first Death with Dignity Act was implemented in Oregon, there has been no evidence of misuse or abuse.
They accept the advocate’s word when the evidence in the study from the NIH above proves a whole bunch of problems and abuses. Every single person The Economist quotes supports euthanasia. They conclude with this story critiquing DC putting in tougher safeguards than other states that legalized it.
Mary Klein, a retired journalist who lives in Washington, DC, and has terminal ovarian cancer, said she has sought medical aid-in-dying from five different doctors to no avail. A few have told her that they think palliative care is sufficient. Ms Klein, who watched her stepmother die in a hospital while receiving pain medicine that made her incoherent, disagrees. “No one wants to be in intolerable pain – but just as important is self-determination. I want to die peacefully in my home surrounded by loved ones. I want to be lucid when I say goodbye to my wife.”
Problems with Oregon’s Reporting Laws
On top of the NIH noting the problems with safeguards, the Charlotte Lozier Institute points out the problem with detecting abuses. They note two main reasons that the claim of no abuses in 20 years isn’t trustworthy.
The first problem with that claim is how difficult it is to determine what would constitute an “abuse” under this law. As previously documented, the Oregon statute and its imitators are artfully filled with loopholes. Physicians, witnesses, and others involved in the process need not comply objectively with the law’s requirements, but only show “good faith” compliance, exempting physicians from their usual obligation not to be negligent. The prescribing physicians need not refer a patient for psychological evaluation even in a clear case of clinical depression — such referral is required only if the doctors think the patient’s depression causes “impaired judgment.” So if they agree with the patient’s judgment that he or she is better off dead, there is no referral. And so on.
The second problem is that the Oregon system is tailor-made to conceal, not reveal, abuses. The physicians involved in prescribing the drugs are the only people allowed to file reports on these cases. The Oregon Health Authority itself says it has no legal warrant to do anything but take this self-reporting at face value. If other doctors found that the patient is not eligible for assisted suicide, patient or family can simply keep trying other doctors until they find one ardently committed enough to assisted suicide to sign the forms – and it is only that last doctor who files a report. So the very cases that most cry out for investigation – in which other doctors had concluded that this patient is not eligible to receive lethal drugs – are those in which the only report is most likely submitted by ideologically committed physicians inclined to ignore or conceal problems. Those physicians are then told by the state to falsify the death certificate, listing the underlying illness as cause of death, so there will be no autopsy or independent scrutiny. And after filing an annual report from which all identifying information has been removed, the state destroys the original reports.
The Canadian Experience
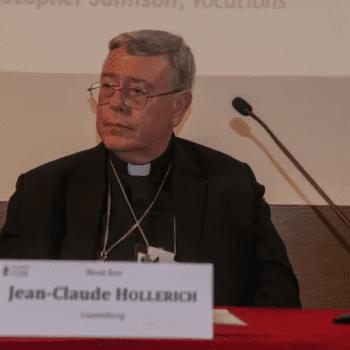
After I finished my first draft, I saw a bishop from Canada tweet a recent story I want to add. Maclean’s (think the Canadian version of TIME or Newsweek) carried a story about the second anniversary of the right to die legislation.
Canadians were asked in 2016 to accept what is now called Medical Assistance in Dying (MAiD) as standard practice in the health-care system. But as the second anniversary of the federal law sanctioning assisted suicide passes this month, ambiguities embedded in the new regulatory regime are turning end-of-life care into a troubling leap of faith for doctors and patients alike. […]
“End-of-life care cannot be limited simply to medical assistance in dying,” Collége President Dr. Charles Bernard writes in a May 29 recently published letter to provincial Health Minister Gaétan Barrette. “That option makes no sense, from a medical point of view, unless it is part of a robust and complete system of palliative care in Quebec.” […]
“In certain identified cases, patients, for the lack of (palliative) care, might have had no choice but to ask for medical assistance in dying to end their days ‘in dignity,’ which deeply concerns us,” the Collège president tells the minister.
Worse, he adds, the Collège has been hearing increasing concerns from its member doctors about re-direction of already scarce resources from palliative care to medical assistance in dying, which risks a violation of both the letter and the spirit of Quebec’s law governing end-of-life care.
You can read more on the Maclean’s site as this author outlines several cases. In summary, in Canada, after euthanasia was legalized, palliative care diminished to the point euthanasia seems like the only option.
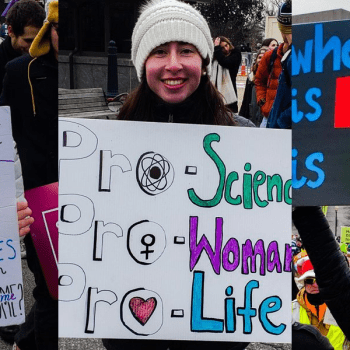
Why We Must Say “NO!” to Euthanasia and Assisted Suicide
Euthanasia and assisted suicide are evil and immoral. God is the Lord of life! However, they are also subject to the problem of increasing evil in how they happen. When depressed patients die from them, or euthanasia lacks full conscious consent, we have something even worse. It is a form of widespread killing.
Euthanasia and assisted suicide should never happen. There are three ways we can prevent them. First, keep them illegal. Second, if they are legal, make sure the safeguards are in place and there are serious consequences that the DA prosecutes for those not following every letter to protect people against assisted suicide or euthanasia. Finally, we need to give people hope and convince them their life is worth living.
Pope Francis talked about how we do evil “with white gloves” regarding abortion but this also applies to euthanasia. We need to respect all life and should not kill off the elderly or disabled with such practices. Allowing euthanasia seems to lead inevitably to a slippery slope where we do evil with white gloves.
UPDATE: I published another article on this slipery slope with new stories.